Table of Content
- 1. Why “Sterile Conditions” Do Not Guarantee Contamination-Free Results
- 2. What Sterile Technique Actually Controls
- 3. Hidden Sources of Contamination in Microbiology Labs
- 4. How to Systematically Identify the Source of Contamination
- 5. How to Systematically Identify the Source of Contamination
- 6. Conclusion
In day-to-day microbiology work, contamination is often recognized not through a single dramatic failure, but through recurring, difficult-to-explain inconsistencies. Plates that were clean in previous runs begin to show unexpected colonies, negative controls occasionally fail, and results that once appeared stable become harder to reproduce. These issues tend to emerge gradually, even in laboratories where sterile techniques are well established and routinely applied.
In an earlier article, Why Perfect Bacterial Culture Is Hard to Achieve in the Lab: Key Challenges, we discussed the broader difficulties of maintaining ideal conditions for microbial growth. Many of those challenges are closely linked to contamination, particularly when its sources are subtle rather than obvious.
This article focuses on common contamination source issues in microbiology laboratories, drawing on patterns frequently encountered in routine experimental work. Rather than attributing contamination to isolated mistakes, it examines how everyday practices, environmental factors, and workflow habits can collectively contribute to persistent contamination problems.
1. Why “Sterile Conditions” Do Not Guarantee Contamination-Free Results
In microbiology laboratories, the term sterile conditions is often used to describe a controlled experimental environment. However, sterility in this context does not represent an absolute state. Instead, it refers to a set of practices designed to reduce the probability of microbial introduction, not to eliminate all possible sources of contamination.
A key reason contamination persists is that sterile techniques primarily control direct and identifiable risks, such as contact with non-sterile surfaces or exposure to known contaminants. They are less effective at managing indirect, time-dependent, or behavioral factors that are inherent to routine laboratory work. As a result, experiments may still become contaminated even when established protocols are followed correctly.
Another important limitation is that sterile conditions are often defined under ideal assumptions. Standard operating procedures are typically developed to represent best-case scenarios: stable environments, consistent workflows, and uniform operator behavior. In practice, laboratory conditions vary continuously. Small deviations—such as brief exposure during handling, changes in airflow, or variations in operator timing—can cumulatively increase contamination risk without violating any explicit rule.
It is also important to recognize that sterility is not uniformly maintained throughout an experiment. Many microbiology workflows involve multiple steps performed over extended periods. Each step introduces a new opportunity for microbial entry, particularly when materials are repeatedly handled, opened, or transferred. Even minor lapses in temporal control can have measurable effects on experimental outcomes.
Finally, sterile conditions do not account for probabilistic events. Contamination does not always occur immediately or visibly. Instead, it may arise sporadically, becoming apparent only after incubation or replication. This probabilistic nature explains why contamination can appear inconsistent or random, despite similar handling and controlled environments.
Sterile conditions reduce risk but do not remove it entirely. Understanding their limitations is essential for interpreting unexpected results and for identifying contamination sources that fall outside conventional definitions of sterility.
2. What Sterile Technique Actually Controls
Sterile technique in microbiology refers to a set of laboratory practices designed to minimize the introduction of unwanted microorganisms into experimental systems. At its core, sterile technique focuses on observable contact and direct transfer risks. It addresses aspects of work where contamination can be reasonably predicted and visibly controlled.
For example, sterile technique effectively controls:
-
Contact with non-sterile surfaces
Avoiding direct touch of sterile instruments, culture media, or open vessels with hands or other non-sterile objects. -
Cross-contamination between samples
Using separate sterile tools for each sample, changing pipette tips, and avoiding reuse of open instruments. -
Handling of reagents and media under controlled conditions
Pouring media in a clean environment, using flame or filtered hoods during transfers, and preventing airborne droplets from directly entering sterile vessels. -
Visible and immediate exposure risks
Such as leaving a plate uncovered while working, or placing sterile materials near obvious sources of contamination.
While sterile technique is effective for these aspects, it does not control all sources of contamination, especially those that are indirect, cumulative, or subtle in nature. Key limitations include the following:
-
Airflow dynamics and micro-aerosols
Even in laminar hoods or clean benches, unpredictable air currents and turbulent eddies can carry microorganisms to surfaces that are technically maintained as “sterile.” -
Time-dependent exposure
Sterile materials may remain “uncontaminated” at the moment of handling, but repeated exposure over time—such as extended work on an open culture or multiple transfers—creates cumulative risk not addressed by sterile technique alone. -
Behavioral and procedural micro-movements
Minor actions such as repositioning hands, adjusting glasses, or shifting instruments introduce contamination risks that are difficult to capture in protocol checklists, yet are common in real workflows. -
Environmental and background microbiota
Sterile technique presupposes that environmental microflora can be excluded, but organisms residing on equipment surfaces, in ventilation systems, or on nearby materials can influence outcomes without direct human contact.
Understanding what sterile technique does and does not control allows laboratory personnel to better interpret contamination events. Rather than assuming unanticipated contamination implies procedural error, it is more useful to consider whether the source was beyond the specific risks that sterile technique was designed to mitigate.

3. Hidden Sources of Contamination in Microbiology Labs
Many contamination events do not originate from clear procedural violations, but from subtle factors embedded in routine laboratory work. These hidden sources often introduce intermittent risk, making contamination difficult to trace and results harder to reproduce.
3.1 Human Behavior and Micro-Movements
Human involvement is an unavoidable component of most microbiology workflows, and even experienced laboratory personnel introduce variability through small, often unconscious actions. These micro-movements—minor adjustments, brief pauses, or habitual gestures—can create contamination risks that are not captured by standard protocols.
One common example is hand repositioning during sample handling. While gloves are worn and instruments are sterile, subtle movements such as adjusting grip, shifting posture, or reaching across the workspace can momentarily alter the spatial relationship between sterile materials and potential contamination sources. These movements may briefly expose open containers or disrupt controlled airflow without being perceived as errors.
Another factor is task-related distraction. During repetitive procedures, attention often shifts toward efficiency or downstream steps rather than immediate exposure risk. Actions such as pausing with an open tube, holding a pipette tip mid-air while checking labels, or setting tools down temporarily can extend exposure time in ways that are difficult to quantify but biologically relevant.
Experience can also contribute to risk through habitual optimization. As techniques become routine, individuals may streamline movements or omit steps they perceive as low-risk. While this often improves efficiency, it can also reduce adherence to protective margins built into protocols, especially under time pressure or high workload.
Importantly, these behaviors do not reflect negligence or poor training. They are a natural consequence of human interaction with complex manual tasks. Recognizing human micro-movements as a contamination factor allows laboratories to shift focus from individual fault to workflow design, spatial awareness, and time management, all of which play a critical role in contamination control.
3.2 Airflow, Lab Layout, and Environmental Exposure
Airborne contamination is often underestimated because it is largely invisible and difficult to associate with a specific action. While microbiology laboratories are designed to limit environmental exposure, airflow behavior within real working spaces is rarely uniform or static, and this variability can directly influence contamination risk.
Sterile technique assumes relatively stable airflow conditions, particularly when work is performed in biosafety cabinets or laminar flow hoods. In practice, airflow can be disrupted by routine factors such as personnel movement, opening and closing doors, nearby equipment operation, or even subtle changes in room pressure. These disturbances may generate localized turbulence, allowing airborne microorganisms to settle onto open surfaces or culture vessels without direct contact.
Laboratory layout also plays a significant role. The proximity of workstations, incubators, waste containers, and shared equipment can create unintended exposure pathways. For example, performing open culture work near high-traffic areas or frequently accessed storage spaces increases the likelihood of airborne transfer, even if sterile technique is otherwise maintained. Over time, these environmental contributions can lead to sporadic contamination events that are difficult to reproduce or trace.
Environmental exposure is further influenced by background microbial load, which varies between laboratories and even within different zones of the same lab. Surfaces that are not directly involved in experimental work—such as benches, instrument exteriors, or shelving—can act as reservoirs for microorganisms that become mobilized through airflow or vibration. Because these sources are indirect, they are often overlooked during contamination investigations.
Importantly, airflow- and environment-related contamination rarely produces immediate or consistent failure. Instead, it introduces probabilistic risk, where contamination appears intermittently despite similar experimental handling. Recognizing the influence of airflow and lab layout shifts the focus from individual technique alone to the broader experimental environment in which sterile work is performed.
3.3 Handling Habits: The Human Factor in Contamination
We often treat certified sterile consumables as “set and forget” items, yet the human hand is the most frequent source of contamination in the lab. It’s the subtle, day-to-day habits—not manufacturing flaws—that usually compromise a workflow.
The risk often starts with shared stock bottles. Every time a common buffer is opened, the clock resets on its purity. In a busy lab, airborne microbes find easy entry points, leading to a slow-burning contamination that might only surface during a critical, long-term incubation. Aseptic discipline also tends to erode under pressure. “Efficiency-driven” habits, like resting a pipette tip near a non-sterile sleeve or hovering over an open flask, are enough to introduce trace impurities that skew sensitive data.
Even the way we stage materials matters. Placing sterile kits in the same footprint as non-sterile samples or setting a lid down on the bench “just for a second” creates indirect contamination routes. These issues are further masked by poor storage practices—reusing reagents across different experiments or ignoring the degradation caused by repeated thawing. Because these contaminants don’t always turn the media cloudy overnight, they persist unnoticed, quietly ruining the reproducibility of the research. In short, sterility is a fragile condition, not a permanent attribute; it is maintained by how we move, not just what we buy.
3.4 The Hidden Dynamics of Cross-Contamination
While overt contamination is easy to spot, cross-contamination between parallel experiments is a far more subtle variable that often goes undetected. It thrives in the gaps between well-controlled procedures, appearing not as a sudden catastrophe but as a persistent source of experimental “noise.”
Much of this risk stems from the sheer complexity of modern lab schedules. Processing diverse cultures side-by-side—each with its own growth rate and resistance profile—invites trouble. A brief lapse in focus during a high-throughput session or the habit of keeping tubes uncapped for convenience can trigger a transfer event that is impossible to trace. This issue is compounded when labs rely on shared infrastructure. Without a clear “temporal buffer” between different experimental runs in the same biosafety cabinet or incubator, the microbial footprint of a previous user can easily influence the next set of results.
Perhaps the most overlooked culprits are the “non-critical” tools: the vortex mixers, centrifuge adapters, and shared timers that move freely between benches. These items are seldom cleaned with the same intensity as primary instruments, allowing them to serve as vehicles for cross-talk between projects. Because the impact is often subclinical—manifesting as a slight shift in growth curves or unexpected background growth rather than a total loss of samples—cross-contamination can persist for months, quietly undermining the integrity of long-term datasets.

4. How to Systematically Identify the Source of Contamination
Identifying a contamination source is less about finding a “smoking gun” and more about understanding the ecology of your lab space. It’s a transition from reactive damage control to proactive system analysis.
When you first spot an unexpected growth, resist the urge to throw it away immediately. That contaminated plate is actually a data point. Does the morphology look like skin flora? Is it a hardy mold or a fast-growing bacillus? Recording these details before you sanitize the area is crucial. If you destroy the evidence too early, you’re doomed to repeat the mistake.
The next phase is isolation. You have to stop assuming that any component—even a brand-new bottle of media—is beyond suspicion. By systematically swapping out one variable at a time, you can often find that the leak isn’t coming from where you’d expect, but from a “blind spot” in the workflow, like a shared vortexer or a contaminated incubator seal.
We also have to be brutally honest about how we actually work. Lab habits tend to evolve toward the path of least resistance. Under high throughput, we might start hovering over open bottles or skipping a glove change without even realizing it. These aren’t intentional errors; they are efficiency-driven shortcuts. Systematic troubleshooting means looking past the idealized protocol and examining the real-world “muscle memory” of the team.
Environmental factors like air quality or bench layout should be the last pieces of the puzzle. They rarely cause issues in a vacuum; instead, they exploit existing cracks in aseptic technique. In the end, taking the time to truly root out a contamination source isn’t just about saving the next experiment—it’s about building a culture of reproducibility where the data can actually be trusted.
5. How to Systematically Identify the Source of Contamination
Identifying a contamination source is less about finding a “smoking gun” and more about understanding the ecology of your lab space. It’s a transition from reactive damage control to proactive system analysis.
When you first spot an unexpected growth, resist the urge to throw it away immediately. That contaminated plate is actually a data point. Does the morphology look like skin flora? Is it a hardy mold or a fast-growing bacillus? Recording these details before you sanitize the area is crucial. If you destroy the evidence too early, you’re doomed to repeat the mistake.
The next phase is isolation. You have to stop assuming that any component—even a brand-new bottle of media—is beyond suspicion. By systematically swapping out one variable at a time, you can often find that the leak isn’t coming from where you’d expect, but from a “blind spot” in the workflow, like a shared vortexer or a contaminated incubator seal.
We also have to be brutally honest about how we actually work. Lab habits tend to evolve toward the path of least resistance. Under high throughput, we might start hovering over open bottles or skipping a glove change without even realizing it. These aren’t intentional errors; they are efficiency-driven shortcuts. Systematic troubleshooting means looking past the idealized protocol and examining the real-world “muscle memory” of the team.
Environmental factors like air quality or bench layout should be the last pieces of the puzzle. They rarely cause issues in a vacuum; instead, they exploit existing cracks in aseptic technique. In the end, taking the time to truly root out a contamination source isn’t just about saving the next experiment—it’s about building a culture of reproducibility where the data can actually be trusted.
6. Conclusion
Contamination is rarely a “smoking gun” event where one single mistake ruins everything. In the real world, it’s usually a slow build-up—the friction between high-pressure routines, environmental quirks, and those tiny habits we don’t even realize we’ve formed. The goal shouldn’t be just “firefighting” the latest outbreak; it’s about designing a workflow that is resilient enough to handle the chaos of a busy lab.
At GenFollower, we know that great science depends on the small things. We don’t just manufacture consumables; we build tools that help you take control of your experimental variables. We believe that a better understanding of the “why” behind lab failures makes for better research.
If you’re looking for more than just a product catalog—if you want practical, no-nonsense insights into the challenges we all face at the bench—we invite you to check out our News & Blogs section. Let’s stop chasing contamination and start preventing it together.
Recent Posts
Common Contamination Source Issues in Microbiology Labs
In day-to-day microbiology work, contamination is often recognized not through a single dramatic failure, but through recurring, difficult-to-explain inconsistencies. Plates that were clean in previous runs begin to show unexpected colonies, negative controls occasionally fail, [...]
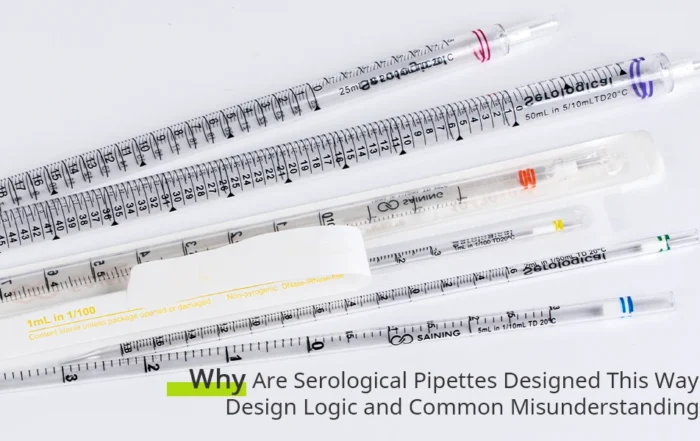
Why Are Serological Pipettes Designed This Way? Design Logic and Common Misunderstandings
Serological pipettes are part of everyday life in many laboratories. Whether transferring culture media, handling large liquid volumes, or supporting routine cell culture work, they are often picked up almost without thinking. Their shape, [...]
Plate Heat Sealer FAQs: What Often Goes Wrong and How Labs Fix It
Plate heat sealers are widely used in laboratories to protect samples from evaporation, leakage, and contamination. However, in daily use, many labs encounter recurring issues—inconsistent seals, unclear parameter settings, compatibility questions, or unexpected sealing [...]